Ankle Sprain (Child)
An ankle sprain is a stretching or tearing of the ligaments that hold the ankle joint together. While a child can have both a broken bone and a sprain, your child has no broken bones.
An ankle sprain is a common injury for both children and adults. It happens when the ankle turns, twists, or rolls in an awkward way. This can be caused by a sports injury, or doing something as simple as stepping on an uneven surface.
Ligaments are made of tough connective tissue. Normally, ligaments stretch a certain amount and then go back to their normal position. A sprain happens when a ligament is forced to stretch more than the normal amount. A severe sprain can actually tear the ligaments. If your child has a severe sprain, there may have been something like a pop when the injury occurred.
Ankle sprains are given a grade depending on whether they are mild, moderate, or severe:
-
Grade 1. A mild sprain with minor stretching and damage to the ligament.
-
Grade 2. A moderate sprain where the ligament is partly torn.
-
Grade 3. The most severe kind of sprain. The ligament is completely torn.
Most sprains take about 4 to 6 weeks to heal. A severe sprain can take several months to recover.
Your child’s healthcare provider may order X-rays to be sure there is no fracture or broken bone.
The injured area will feel sore. Swelling, stiffness, and pain may make it hard to walk. Your child may need crutches if walking is painful. Your child’s provider may have your child use a cast, boot, or air splint. This will depend on the grade of ankle sprain.
Home care
For a grade 1 sprain, use RICE (rest, ice, compression, and elevation):
-
Rest the ankle. Your child should not walk on it until their healthcare provider says it's OK.
-
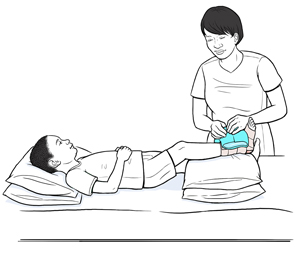
Use ice packs right away to help control swelling. Place an ice pack over the injured area for 20 minutes. Do this every 3 to 6 hours for the first 24 to 48 hours, or as directed. Keep using ice packs to ease pain and swelling as needed. To make an ice pack, put ice cubes in a plastic bag that seals at the top. Wrap the bag in a clean, thin towel or cloth. Never put ice or an ice pack directly on the skin. The ice pack can be put right on the cast, bandage, or splint. As the ice melts, be careful that the cast, bandage, or splint doesn’t get wet. If your child has a boot, open it to apply an ice pack, unless told otherwise by the healthcare provider.
-
Compression devices help to control swelling. They also keep the ankle from moving and support the injured ankle. These devices include dressings, bandages, and wraps.
-
Elevate the injured leg above the level of your child's heart as often as possible.
-
A child 1 year and older can prop their leg on a pillow while sitting or sleeping.
-
A baby younger than 12 months who is awake and observed can be placed on their side with the injured leg elevated. If your baby falls asleep, move them to a flat, firm surface. Never use pillows for sleep or put your baby to sleep on their stomach or side. Babies younger than 12 months should sleep on a flat surface on their back. Don't use car seats, strollers, swings, baby carriers, and baby slings for sleep. If your baby falls asleep in one of these, move them to a flat, firm surface as soon as you can.
-
If your child has a grade 2 sprain, follow the RICE guidelines. This type of sprain will take longer to heal. Your child may need a splint, cast, or brace to keep the ankle from moving. Follow the healthcare provider's instructions on how long your child needs to wear the splint, cast, or brace.
-
If your child has a grade 3 sprain, they may be at risk for long-term ankle instability. In rare cases, surgery may be needed. Your child may need to wear a short-leg cast or a walking boot. Follow the provider's instructions on how long your child needs to wear the cast or walking boot.
-
After 48 hours, it may be helpful to apply heat for 20 minutes several times a day. You can do this with a heating pad or warm compress. Or you may want to go back and forth between using ice and heat. Never put heat directly to the skin. Always wrap the heating pad or warm compress in a clean, thin towel or cloth.
-
You may use over-the-counter (OTC) pain medicine such as acetaminophen to control your child’s pain unless another pain medicine was prescribed. OTC medicines also include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen. Don't give your child aspirin. Taking aspirin can put them at risk of getting Reye's syndrome. Don’t give ibuprofen to a child younger than 6 months old. Always talk with your child’s provider before using these medicines if your child has chronic liver or kidney disease. Also, talk with the provider if your child has ever had a stomach ulcer or digestive bleeding.
-
Have your child do any exercises from the provider, as directed. These can help your child be more flexible and improve their balance and coordination. This helps prevent long-term ankle problems.
Prevention
To help prevent ankle sprains, it’s important to have good strength, balance, and flexibility. Check that your child:
-
Always warms up before playing sports, exercising, or doing something very active
-
Is careful when walking or running on uneven or cracked surfaces
-
Wears shoes that are in good condition and fit well
-
Listens to their body’s signals to slow down when in pain or tired
Follow-up care
None of the X-rays your child had today show any broken bones, breaks, or fractures. Sometimes fractures don’t show up on the first X-ray. Bruises and sprains can sometimes hurt as much as a fracture. These injuries can take time to heal completely. If your child's symptoms don’t get better or they get worse, talk with your child's healthcare provider. Your child may need a repeat X-ray.
Follow up with your child’s healthcare provider as advised. Your child may need to see an orthopedic or bone doctor for further evaluation.
When to get medical advice
Call your child's healthcare provider right away if any of these occur:
-
Fever (see "Fever and children" below)
-
Chills
-
The injury doesn't seem to be healing
-
The swelling comes back
-
The cast or splint has a bad smell
-
The plaster cast or splint gets wet or soft
-
The fiberglass cast or splint gets wet and does not dry for 24 hours
-
The pain or swelling increases, or redness appears
-
The toes become cold, blue, numb, or tingly
-
The pain doesn’t get better, or it gets worse. Babies may show pain as crying or fussing that can’t be soothed.
-
Your child has trouble moving the injured ankle
-
The skin looks blue, purple, or gray (discolored), has blisters, or is irritated
-
The ankle is re-injured
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
Fever readings for a child aged 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° F (38° C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older