Well-Child Checkup: 4 Months
|
At this age I will begin to interact more with my environment. I am learning to roll over (usually tummy to back first). I have discovered my hands. I soon learn to put my hands in my mouth, and then I try grasping objects with my hands. I like to hold rattles and squeaky toys and those with different textures and shapes. I will start to make different noises with my voice and begin to laugh and drool.
Please remember to:
Always use my car seat. Watch what I can reach or grasp because everything will go to my mouth, and I can choke or eat something poisonous. Give me toys that are unbreakable, have no small parts or sharp edges, and are too large to swallow. I’ll be able to roll soon, so never leave me near an edge where I might fall. If I’m in a carrier, put me on the floor or in my crib, because I will bounce and rock, and I could tip the carrier over. Put me to sleep on my back and put me down in my bed when I am still awake so I can learn to put myself to sleep.
Feeding Solid Foods to Your Baby
At four months of age, once your baby has good head control, you can start introducing solid foods. This should be an enjoyable time for you and your baby. Feeding and meals in general should be a pleasant time for the whole family, free from tension and conflict. Children, like adults, have variations in appetite from day to day and variations in taste preference. However, if offered a balanced diet, a baby will select a nutritious variety over several weeks (not necessarily each day). This is not true if a baby is being offered empty calories like cookies, sweets, juice, or other junk food. It is important to remember that food is a source of nutrition and not a pacifier for a cranky baby or a means of quieting an active toddler.
Here are some basic guidelines to help ensure a successful feeding experience:
-
At this age, breastmilk or formula should still be your baby’s main source of nutrition. If your baby is due to nurse or have a bottle before a solid meal, do that first before offering solids. Continue breastfeeding until one year of age or longer; continue formula until one year of age, at which point you can offer 2-3 cups per day of whole milk instead.
-
All babies need vitamin D supplements to protect their bones and electrolytes. Formula companies add it for you, so if your baby is taking 16 ounces per day of formula, he is getting adequate vitamin D from that. If your baby is breastfed, continue daily vitamin D (400-600 units, or 1 dropper of D-Vi-Sol or Poly-Vi-Sol daily).
-
Start your baby’s solid food experience with a positive attitude. Most babies at this age are eager to explore new tastes and will enjoy eating. But if your baby balks on the first day, don’t try to force the issue or force-feed your baby. Generally, after several days, your baby will become more enthusiastic about eating. It may take 10 or 20 repetitions of tasting one food before your baby starts to like it, so keep trying!
-
Make sure all foods that you offer are puréed so your baby won’t choke on them. You can easily make baby food by puréeing some of what you’re eating; you may need to add a little water to make the consistency right for your baby. Start by offering foods with watery consistency, and gradually thicken as tolerated.
-
Offer solid foods 2-3 times per day at first, and gradually increase to three solid meals per day. Start with just a few spoonfuls of food and increase the amount over several meals. Do not continue feeding if your baby shows signs of resistance. Babies will stop eating when they’re full.
-
You can start by offering any food, but a good first food is rice cereal, which is a powder that you can find in the baby food section of the grocery store. Put an ounce of expressed breastmilk, formula, or water in a bowl, then stir in rice cereal powder until the cereal is the consistency of watery oatmeal. Most babies like rice cereal because it tastes like something they’re familiar with (breastmilk or formula). Rice cereal is also fortified with iron, which most babies (especially breastfed babies) start to get low on around this age. Offering rice cereal once a day can be an excellent addition to your baby’s diet.
-
The only foods that are off-limits to offer to an infant are honey (which can cause botulism) or foods a baby can choke on. We used to think that withholding the more common allergy foods (like eggs, dairy, wheat, strawberries, soy, nuts, peanut butter, shellfish, etc.) would lead to fewer food allergies. In fact, delaying the introduction of these foods seems to lead to more allergies. It’s fine to introduce these highly allergenic foods, starting in small amounts, once other foods like vegetables and grains are tolerated. New allergenic foods can be tried every few days. For all other foods, there’s no need to wait several days between new foods because delaying introducing foods just leads to deficient nutrition. Make sure any food you offer is puréed so your infant will not choke on it, but otherwise you can and should offer any food other than honey. Foods with multiple ingredients are fine. Spices are fine, and introducing foods with different flavors now will help your child like them later. You can easily make your own baby food by puréeing some of your own meal in a blender!
-
When you start introducing solid foods, you can introduce water in a sippy cup. Water helps rinse teeth, flush the kidneys, and reduce constipation. Using a cup for water also teaches a new skill.
-
Allow your baby to feed himself. At first he will not be coordinated enough to get an adequate amount of food into his mouth. But letting him try to self-feed is really good for developing fine motor skills and healthy eating habits. You may have to give him a bath after meals, but it’s worth it!
-
Remember that fruit is healthy, but juice is a junk food! Please try to avoid giving juice or limit it to 4 ounces per day. Also avoid other sweets and junk food.
-
Avoid hard or compressible food like round candies, nuts, popcorn, peas, etc., because your baby can choke on them.
-
You can offer your baby organic food, but studies have not yet shown that it’s better than regular food. Organic and non-processed food (if pasteurized when necessary and stored appropriately) certainly aren’t worse than regular food, though, so if you have the money and desire to eat organic, go for it.
Smile! Your Baby's About to Start Teething!
Teething is an exciting milestone, but it can also be a challenging time. Teething infants tend to drool a lot, chew on everything they can get their hands on, and often become fussy and have interrupted sleep as the teeth are about to erupt.
The Teething Process:
All children are different, and there's a great variability in the timing of teething and the symptoms babies feel. As a general guideline, though:
-
The teething process usually starts at about three months of age. You may notice excessive drooling at this point.
-
In general, the first teeth begin to erupt at approximately 6 months of age, and babies generally get a couple of new teeth each month, finishing teething by about three years of age.
-
There are 20 primary ("baby") teeth. From middle to back, these are the central incisors (front teeth), lateral incisors, canines, first molars, and second molars. The first teeth to erupt are usually the lower front teeth (central incisors), followed by the upper front teeth (central incisors). Next come the upper and lower lateral incisors, then the first molars, then canines, and finally the second molars. Keep in mind that all children are different and timing (and tooth eruption order) for any individual child may vary, so don't worry if your child doesn't follow these steps exactly.
Symptoms of Teething:
Contrary to popular myths, teething does not cause fever. It does cause:
-
Drooling, which may cause chin rash due to excessive moisture
-
Chewing on or biting fingers or toys
-
Swollen, tender gums
-
Fussiness (due to gum soreness) and sleep interruption for 3-5 days before teeth erupt
How to Relieve Discomfort of Teething:
-
Give your baby something cool to chew on, like a teething ring, a chilled washcloth, or a regular-sized (not baby-sized) chilled carrot. Do not put teething rings in the freezer or give your baby ice to chew on because this can freeze and damage gums.
-
Use a clean finger or cold teething ring to gently rub your baby's gums for a couple of minutes at a time.
-
If nothing else is working, give your baby a pain relief medicine like acetaminophen (Tylenol) or ibuprofen (Advil or Motrin). Infants should not be given ibuprofen until they are six months old.
-
Do not use teething gels. They can be harmful because your baby may bite down on or otherwise damage numb gums, causing more pain later on. Also, if excessive amounts of teething gels are swallowed, they can lead to throat numbness causing difficulty swallowing or breathing.
Don't forget to brush!!
Once your baby has teeth, make sure to brush them twice a day with a soft infant toothbrush, or wipe them with a washcloth. When your infant is older, you can use an infant/toddler toothpaste to help your child cooperate with brushing. Don't let your baby go to bed with a bottle, because this leads to cavities. The American Dental Association (ADA) and the American Academy of Pediatrics (AAP) recommend the first dentist visit at one year of age.
Fever in Children
What Is Fever?
Fever is the body’s normal response to
infections and may be helpful in fighting them. When white blood cells attack germs, they release chemical signals which cause the brain to elevate the temperature. This elevation may help the body kill the germs faster. The usual fevers (100°F to 104°F) that all children get are not harmful. Most are due to viral illnesses; some are due to bacterial ones. Teething does not cause fever.
The symptoms and characteristics of fever include a rectal temperature over 100.4°F (38.0°C), oral temperature over 100°F (37.8°C), and axillary (armpit) temperature over 99°F (37.2°C). While the body’s average temperature is 98.6°F (37°C), it fluctuates from a low of 97.6°F in the morning to a high of 100°F in the late afternoon. Mild elevations of temperature can be caused by exercise, excessive clothing, hot weather, or warm food or drink. If you suspect one of these causes, retake the temperature after 30 minutes.
How Do You Take Temperatures?
Use digital, not mercury, thermometers because they are safer, faster, and more accurate. For children under five years of age, use axillary or rectal measurements. Most children four or five and older are ready for oral readings. Ear thermometers may be unreliable, especially in children under one year old. In young children, high ear thermometer readings should be confirmed by another method.
Axillary: Place the tip of the thermometer in a dry armpit and close the armpit by holding the elbow against the chest. If you’re uncertain about the result, check it with a rectal thermometer.
Rectal: Place your child stomach-down on your lap, or on his back on a changing table. Lubricate the end of the thermometer and the opening of the anus with petroleum jelly (Vaseline or KY Jelly). Carefully insert the thermometer about one inch, but never force it. Hold the child still and rest your hand on the buttocks to stabilize the thermometer.
Oral: Be sure your child has not recently taken a cold or hot drink. Place the tip of the thermometer underneath the tongue on either side, rather than at the front of the mouth. The child should hold it in place with the lips and fingers (not the teeth), keeping the mouth closed and breathing through the nose. If the nose is congested, take an axillary temperature. You do not need to check your child's temperature if he is not sick, or many times a day when he is sick. Remember that the main purpose of temperature-taking is to determine if a fever is present, not to chart its every move.
How Long Does Fever Last?
Most fevers associated with viral illness range
between 101°F and 104°F and last for one to three days. In general, the height of the fever isn’t related to the seriousness of the illness. What counts is how sick your child acts. With most infections, the level of fever bounces around for two or three days. Shivering or feeling cold indicates that the fever has peaked; sweating means it is coming down.
It is important to understand that there is no evidence that fever itself can be harmful unless the temperature exceeds 107°F. Fortunately, the brain’s thermostat keeps nearly all untreated fevers below this level. A small number of young children may develop convulsions (seizures) with fever. While these are frightening, they do not appear to cause harm and are not usually a sign of more serious illness. Still, call your child's doctor if your child has a febrile seizure.
When Should I Call?
If your child is under three months old, call us day or night if the rectal temperature is greater than 100.4°F. Beyond three months, call immediately if the fever is over 105°F, your child is crying inconsolably or whimpering, or cries if you touch or move him. Also call immediately if the child’s neck is stiff, any purple spots are present on the skin, breathing is difficult and no better after you clear the nose, or a convulsion (seizure) has occurred. Call if burning or pain occurs with urination. Also call if your child is under two years of age and has a fever of 104°F or greater. Call if the fever has been present more than 72 hours, more than 24 hours without obvious cause, or has returned after going away for more than 24 hours.
Which Medications Should I Use?
Check with our office before using medication for children under four months of age. Children of any age can be given acetaminophen (Tylenol®, Tempra®, Liquiprin®, Panadol®) if the fever is causing discomfort. Acetaminophen will reduce the fever but usually not bring it down to normal and the fever may recur after the aceteminophen wears off. Liquid ibuprofen (Advil, Motrin®) may also help improve comfort and reduce the temperature in feverish children and can be given to infants six months or older. See chart that follows for dosing. If your child is sleeping, don't awaken him for medications, and do not use them for more than three days without consulting your pediatrician.
Other Measures to Take:
Encourage, but don’t force, extra fluids.
Popsicles and iced drinks may help replace body fluids lost because of sweating. Keep clothing to a minimum because most heat is lost through the skin. Bundling up your child will cause a higher fever. Be especially careful of infants, who cannot undress themselves if they become overheated. If your child feels cold or is shivering, use a light blanket. Discourage vigorous activities because they produce additional heat. Normal play, however, is perfectly fine.
A Word of Caution About Aspirin
The American Academy of Pediatrics and other health organizations have recommended that patients through 21 years of age not receive aspirin if they have chickenpox or influenza (any cold, cough, or sore throat symptoms). Several studies have linked aspirin to Reye’s syndrome, a severe illness that resembles encephalitis. Many pediatricians have stopped using aspirin for fevers associated with any illness because it has the potential to be so dangerous.
Medicines and Dosages to Reduce Pain and Fever
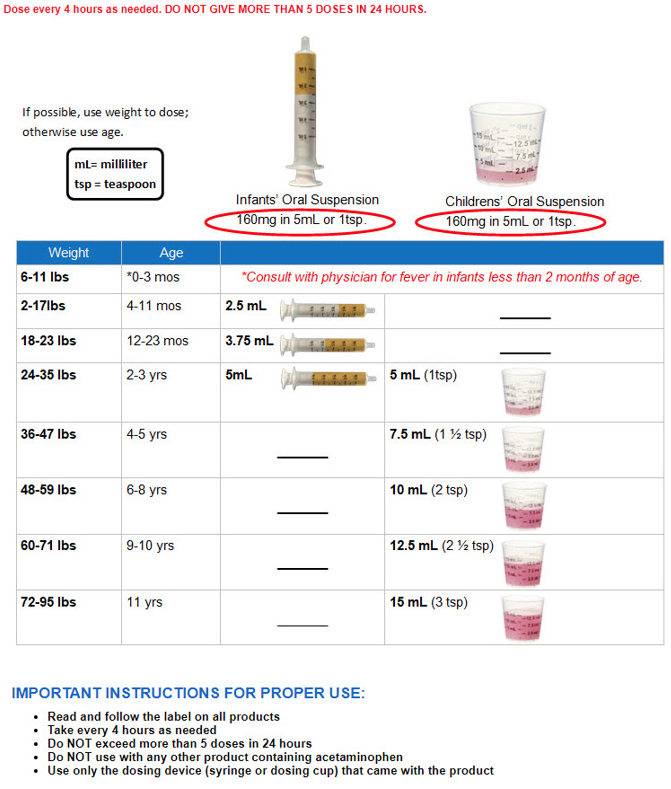
Choose the proper medicine, and measure the dose accurately
-
Always use a proper measuring device. For example: When giving acetaminophen liquid (e.g., Tylenol), use the device enclosed in the package. If you misplace the device, consult your healthcare provider or pharmacist for advice. Kitchen spoons are not accurate measures. When giving ibuprofen liquid (e.g., Advil, Motrin), use the device enclosed in the package. Never use a kitchen spoon!
Take these two steps to avoid causing a serious medication overdose in your children
Don’t give your child a larger amount of acetaminophen (e.g., Tylenol) or ibuprofen (e.g., Motrin, Advil) than is shown in the table below. Too much of any of these medicines can cause an overdose.
When you give your child acetaminophen or ibuprofen, don’t also give them over-the-counter (OTC) cough or cold medicines. This can also cause a medication overdose because cough and cold medicines often contain acetaminophen or ibuprofen. In fact, to be safe, don’t give OTC cough and cold medicines to your child unless you talk to your child’s healthcare provider first.
Pediatric Ibuprofen
Dosing Instructions for Infants and Children
Pediatric Acetaminophen
Dosing Instructions for Infants and Children