Instructions for (EBUS) Guided Biopsy and Flexible Bronchoscopy
What is EBUS guided biopsy?
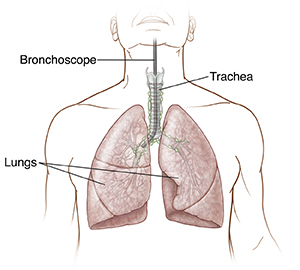
EBUS (Endobronchial ultrasound) is a procedure that uses sound waves through the bronchoscope to visualize and collect tissue samples from your lungs/lymph nodes. It is used along with the Navigational Bronchoscopy for biopsies.
What happens prior to the procedure?
-
Since this procedure is performed using general anesthesia, you will get a call from the Anesthesiology team to go over your medications and other details.
-
You may need to stop medications (especially blood thinners such as Aspirin, Plavix®, Xarelto® or Eliquis®) ahead of time, so please discuss that with the Anesthesia team and us ahead of time.
-
We may also need to get additional imaging and/or labs prior to the procedure to provide the safest procedure.
How do I prepare for the procedure?
-
Please make sure that you have a responsible adult who can escort you home after the procedure. You cannot drive yourself, or take a bus, taxi or shuttle by yourself. Your escort may drive you in a car, or ride with you in a bus, taxi or shuttle.
-
Please do not eat or drink anything after midnight the night before unless instructed otherwise.
What happens after you check in?
-
After you are escorted to the recovery/holding area, a nurse will check your vital signs and insert an intravenous line (IV line) in your arm which we will use to administer medications.
-
The Anesthesiologist will meet with you, and you will have a chance to ask any questions.
What happens during the procedure?
-
You will be deeply asleep and will not feel any pain or discomfort. The Anesthesiologist will monitor you closely during the procedure. A ventilator (breathing machine) that will breathe for you while you are asleep.
-
The doctor will pass the Navigational Bronchoscope into your lungs through the trachea (airway tube). This small, flexible catheter has a camera at the tip and will be guided into the target area using robotic guidance. Once in place, the biopsy is obtained using specially designed tools. Ultrasound guidance is used as needed throughout the procedure.
What happens after the procedure?
-
Once the procedure is completed, the Anesthesiologist will remove the airway tube and you will be moved to the recovery area. Most patients are in recovery for about 2 hours. A nurse will monitor you closely. You may not be able to eat or drink for 2 hours after the procedure.
-
When you are considered ready to go home, the nurse will go over the care you will need at home, remove the IV, and your escort can take you home.
What care should I take at home?
-
You may feel sleepy for the rest of the day and the next morning. Do not drive or use heavy machinery and do not drink alcohol for 24 hours after the procedure.
-
You may notice some sore throat or hoarseness, mild blood-tinged phlegm, low-grade fever for 24 hours after the procedure. If these symptoms persist for more than 24 hours after the procedure, please contact our office.
-
If you notice chest pain, shortness of breath, fast heart rate or cough up more than 1 tablespoon of red blood at any time, please call 911 or go to the Emergency room right away.
When do I have the results?
-
On average, it takes 1-2 weeks for the lab to perform the necessary tests on the samples. You will be contacted as soon as the results are available and if needed, will be scheduled for a follow-up appointment to review them.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Bleeding from your nose or throat
-
Coughing up a large amount of blood
-
A fever above 100.4°F (38°C) for more than 24 hours, or as advised by your provider
-
New symptoms, symptoms that get worse, or symptoms that don't go away
When to call 911
Call 911 right away if you have:
-
Chest pain
-
Severe shortness of breath or trouble breathing
-
Fast heart rate
-
Bluish-colored skin, lips, or mouth