Well-Child Checkup: 15-18 Months
I am pretty mobile now, and I can walk, run, and climb. I like to throw things and chase after them. I also like to pound on things and make loud noises.
Scribbling with crayons, playing with push and pull toys, and stacking rings on a spindle are other activities I enjoy. I am learning to drink from a cup and use a spoon. I can say "Mama" and "Dada" to mean my parents, and I can say a few other words too. I can imitate what other people say. Pretty soon I will be combining two words together to make "sentences." I understand the word "no" and I can understand a lot of other things too, much more than I can say.
Please remember to:
Use my car seat, rear-facing until I am two years old or outgrow the weight or height limits of my car seat. Keep pieces of hard food away. I can easily choke on nuts, chips, grapes, raisins, and hot dogs too. If you haven’t already, discontinue use of my bottles and pacifiers; I do not need them anymore. Offer me healthy food choices: that way, even if I'm a picky eater, I will get enough nutrition. Teach me about discipline in a loving but firm, consistent way. I learn about rules and limit-setting much more easily with positive support than punishment. Brush my teeth twice a day and teach me how to do it, but watch me please. Only use toddler toothpaste, because I haven't learned to spit it out yet. Take me to the dentist for my first visit, if you haven't done that already.
Toilet-Training Basics
Definition
Your child is toilet-trained when, without any reminders, your child walks to the potty, undresses, urinates or has a bowel movement, and pulls up his pants. Some children will learn to control their bladders first; others will start with bowel control. Both kinds of control through the night normally happens several years later than daytime control. The gradual type of toilet training discussed here can usually be completed in two weeks to two months.
Toilet-Training Readiness
Don’t begin training until your child is clearly ready. Readiness doesn’t just happen; it involves concepts and skills you can begin teaching your child at 12 months of age. Reading some of the special toilet-learning books to your child can help. Most children can be made ready for toilet training by 24 months of age and some even by 18 months. If you don't actively try to toilet train your child, by the time she is three years old, she will probably have trained herself, and this is a perfectly fine approach.
The following signs indicate that your child is ready:
-
Your child understands what “pee,” “poop,” “dry,” “wet,” “clean,” “messy,” and “potty” mean. (Teach these words.)
-
Your child understands what the potty is for. (Teach this by having your child watch parents, older siblings, and children near his age use the toilet correctly.
-
Your child prefers dry, clean diapers. (Change your child frequently to encourage this preference.)
-
Your child likes to be changed. (As soon as she is able to walk, teach her to come to you immediately whenever she is wet or dirty. Praise her for coming to you for a change).
-
Your child understands the connection between dry pants and using the potty.
-
Your child can recognize the feeling of a full bladder and the urge to have a bowel movement; that is, he paces, jumps up and down, holds his genitals, pulls at his pants, squats down, or tells you. (Clarify for him: “The poop [or pee] wants to come out. It needs your help”).
-
Your child has the ability to briefly postpone urinating or having a bowel movement. She may go off by herself and come back wet or soiled, or she may wake up from naps dry.
Method for Toilet Training
The way to train your child is to offer encouragement and praise, be patient, and make the process fun. Avoid any pressure or punishment. Your child must feel in control of the process.
Buy supplies.
-
Potty chair (floor-level type). If your child’s feet can reach the floor while he sits on the potty, he has leverage for pushing and a sense of security. He also can get on and off whenever he wants to.
-
Stickers or stars for rewards.
Make the potty chair one of your child’s favorite possessions. Several weeks before you plan to begin toilet training, take your child with you to buy a potty chair. Have your child help you put her name on it. Allow your child to decorate it or even paint it a different color. Then have your child sit on it as a chair. Have your child use it while watching TV, eating snacks, playing games, or looking at books. Keep it in the room in which your child usually plays. Only after your child clearly has good feelings toward the potty chair (after at least one week), proceed to actual toilet training.
Encourage practice runs on the potty. Do a practice run whenever your child gives a signal that looks promising, such as a certain facial expression, grunting, holding the genital area, pulling at his pants, pacing, squatting, squirming, or passing gas. Other good times are after naps or 20 minutes after meals. Say encouragingly, “The poop (or pee) wants to come out. Let’s use the potty.” Encourage your child to walk to the potty and sit there with his diapers or pants off. Your child can then be told, “Try to go pee-pee in the potty.” If your child is reluctant to cooperate, he can be encouraged to sit on the potty by doing something fun, for example, you might read a story. If your child wants to get up after one minute of encouragement, let him get up. Never force your child to sit there. Never physically hold your child there or strap him in. Even if your child seems to be enjoying it, end each session after five minutes unless something is happening.
Praise or reward your child for cooperation or any success. All cooperation with these practice sessions should be praised. For example, you might say, “You are sitting on the potty just like Mommy,” or “You’re trying really hard to put the pee-pee in the potty.” If your child urinates into the potty, she can be rewarded with small presents or stickers, as well as praise and hugs. Although a sense of accomplishment is enough for some children, others need rewards to stay focused. Big rewards (such as going to the ice cream store) should be reserved for when your child walks over to the potty on her own and uses it, or when your child asks to go there with you and then uses it. Once your child uses the potty by herself two or more times, you can stop the practice runs. For the following week, con- tinue to praise your child frequently for dryness and using the potty. (Note: Practice runs and reminders should not be necessary for more than one or two months.)
Change your child after accidents. Change your child as soon as it’s convenient, and respond sympathetically. Say something like, “You wanted to go pee-pee in the potty, but you went pee-pee in your pants. I know that makes you sad. You like to be dry. You’ll get better at this.” If you feel a need to be critical, keep to mild verbal disapproval and use it rarely (for example, “Big boys don’t go pee-pee in their pants,” or mention the name of another child he likes who is trained); then change your child into a dry diaper or training pants in as pleasant and
non-angry a way as possible. Never use physical punishment, yelling, or scolding. Using pressure or force can make a two-year-old child completely uncooperative. Do not keep your child in wet or messy pants for punishment.
Introduce training pants after your child starts using the potty. Switch from diapers to training pants after your child is cooperative about sitting on the potty chair and passes about half of her urine and bowel movements there. She definitely needs training pants if she comes to you to help her take off her diaper so she can use the potty. Take your child with you to buy the underwear and make it a reward for her success. Buy loose-fitting ones that she can easily lower and pull up by herself. Once you start using training pants, use diapers only for naps and nighttime.
Talk with Your Child's Doctor If:
-
Your child won’t sit on the potty or toilet.
-
Your two-and-a-half-year-old child is negative about toilet training.
-
You begin to use force or punishment.
-
Your child is over three years old and not daytime toilet trained.
-
The approach described here isn’t working after two months.
-
You have any other questions or concerns.
Recommended Reading
Joanna Cole: The Parents’ Book of Toilet Teaching, Ballantine Books, N.Y., 1983.
Vicki Lansky: Koko Bear’s New Potty, Bantam Books, N.Y., 1986.
Alison Mack: Toilet Learning, Little, Brown, Boston, 1978.
The Common Cold in Children
What is it?
The cold is by far the most common illness of infancy and childhood. Another name for the common cold is an upper respiratory infection (URI). On average, children get 10 colds per year, often back-to-back in the fall and winter.
What causes it?
At last count, over 100 different viruses have been implicated and isolated as causes of the common cold. A cold is a viral infection that causes inflammation of the linings of the nose, throat, and larynx (voice box). This inflammation results in swelling of these linings and an outpouring of fluids and mucus.
How do you catch it?
A baby or child does not catch a cold by going outside the house or by being in a draft or by a blanket falling off or by not being dressed warmly enough. Colds are contracted from someone else who has a cold. Colds are usually transmitted via “droplet spray," for example by coughing or sneezing. Colds are very contagious.
What are the characteristics of a cold?
The main symptoms of a cold are runny nose and watery eyes. The nose may become plugged by the mucus; this can cause a baby to breathe noisily. Some of the fluid and mucus drains down the throat causing irritation and frequently stimulating a cough. As an additional response to the infection, it is not unusual for the child to develop a low-grade fever. Sore throats are also common.
How long does a cold last?
The average duration of a common cold is 7 to 10 days. The younger child may experience 6 to 10 colds a year. It is not unusual for several of these infections to occur almost one after another. The first year in school (daycare or kindergarten) is notorious in terms of the large number of colds acquired. This is due entirely to an increased exposure to other children with colds. Likewise, a large family means more exposure and consequently more colds. Exposure to colds in the early years is good for the immune system.
Treatment:
There is no specific prevention, treatment or cure for the common cold. There is no solid scientific evidence demonstrating that high doses of vitamin C or zinc or any other supplement either prevent or cure the cold. Antibiotics do not help with cold symptoms or make colds get better faster, and often have severe and even life-threatening side effects. The best we can do is to help relieve the symptoms of the cold while allowing it to take its natural course, and to assure you that complications are not occurring.
-
Fever: Fever is not a disease; it is simply a sign that there is an infection somewhere in the body. Fever itself is not dangerous; rather, it can be beneficial both in helping to eliminate the infecting organism and enabling us to follow the progress of the infection. Fever can be lowered (not eliminated) by appropriate doses of acetaminophen (Tylenol) or ibuprofen (Advil, Motrin), though ibuprofen cannot be given to babies under six months old. These medicines can keep the child comfortable, but when the medication wears off, the fever will return. It is important not to overdress the child with fever; lightweight clothing enables the skin to radiate some of the excess heat generated by the body.
-
Runny nose: In the younger child up to nine months, most breathing occurs through the nose and not through the mouth; therefore, it is important to keep the nasal passages clear. Suctioning the fluids and mucous from the nose with a nasal syringe can be quite effective. Saline nose drops (such as Little Noses or Ocean®) can help lubricate the nasal passages and improve the efficiency of nasal suctioning. Oral decongestants are of limited value in relieving the symptoms of the common cold. The benefits are even less noticeable in younger children, and over the counter medications shouldn’t be used without a physician’s instruction in children less than six years old.
-
Cough: Cough with the common cold usually results from drainage of the nasal mucus into the throat and also from the irritation this drainage may cause to the lining of the throat. Efforts directed at relieving the nasal congestion are most helpful in alleviating the cough. Medications are rarely of benefit and shouldn't be used without a physician's instruction in children less than six years old.
-
Fluids: The child with a cold has an increased fluid requirement due to the URI and its accompanying fever. It's important to keep a sick child well hydrated. Water, tea, Pedialyte and juices are fine for this purpose, after six months of age.
-
Solid foods: Appetite is frequently poor in response to the infection. Forced feedings of solids may result in vomiting and should be discouraged. As long as a sick child is staying well hydrated with fluids, not eating solids well for a few days while sick is not dangerous.
-
Environment: Keeping the house cool will help to keep the child comfortable, and if the weather is permissible, the child can go outside without any danger. Increasing the humidity of the house also can be helpful and can be accomplished by using a cool-mist vaporizer or humidifier. This will soothe the inflamed tissues of the nose and throat and may help reduce the cough.
Possible complications:
If the inflammation spreads beyond the nose and throat to the trachea (windpipe), lungs or ears, we are dealing with complications. Among the more common complications are pneumonia and ear infections. Clues to these secondary complications may be:
-
Fever over 102°F (39°C)
-
Painful crying or screaming
-
Excessive irritability
-
Severe continuous cough
-
Difficulty in breathing
Please call this office if you have any questions regarding the management of a cold or the appearance of any of the signs of complications.
Instructions for Parents of Children with Gastroenteritis
Gastroenteritis (or the stomach flu) is an inflammation and irritation of the intestinal tract. It is usually caused by a virus. Occasionally, it may be caused by bacteria or parasites, but viral causes are by far the most common.
Symptoms
The most common symptom is diarrhea.Vomiting may occur with or without diarrhea. Abdominal cramping is also common. Gastroenteritis itself is not dangerous. Most of the time the recovery is uneventful.
Avoid Dehydration
The danger of dehydration exists with vomiting and diarrhea, especially in small children. If the child is losing fluid faster than it can be replaced, dehydration may result. The most reliable symptoms of dehydration are:
-
12 hours without urination,
-
dry mouth, absence of saliva,
-
sunken eyes
-
extreme inactivity, exhaustion, and/or
-
sunken soft spot-on top of the head of infants.
Vomiting and Diarrhea
Viral illnesses do not respond to antibiotics; instead, they run their own course. Medications to relieve the symptoms of vomiting and diarrhea are rarely used in children because of serious side effects. Therefore, the treatment is primarily supportive. The purpose is to rest the intestinal tract for a short period of time while still providing the necessary fluids and salts to prevent dehydration.
Vomiting
If your child is vomiting, you should give nothing by mouth for at least half an hour to give the stomach a rest. After the period of rest, offer a small amount (one to two table- spoons) of clear liquid (follow the clear liquid diet below). Wait one-half hour. If no vomiting occurs, give another two tablespoons. Continue to slowly decrease the time between drinks and to slowly increase the amount of fluid offered. Avoid forcing too much fluid at one time. If vomiting starts again, repeat the above process starting with the stomach rest.
Clear Liquid Diet (No Solids and No Milk) For breastfed infants: Alternate breast- feeding with Pedialyte® to keep the infant hydrated until the vomiting ceases.
-
For other infants: Pedialyte®
-
For older children: Gatorade®, Clear Broth, Tea, flat Coke®, 7-up®, Ginger Ale or water
After there has been no vomiting for a few hours, give the older child a bland diet. Once they can tolerate bland foods without vomiting, if they desire reglar foods, it's ok to try them. Infants who have not yet begun solids can now be given breastmilk or a soy-based formula until the stools are normal.
Does My Child Need A BRAT Diet?
Foods that are high in fat and sugar will not be tolerated as well as complex carbohydrates, lean meats, yogurt, fruits, and vegetables.
We used to recommend the BRAT (bread, rice, applesauce, and toast) diet for diarrheal illnesses, but studies show that this is not necessary and reduces nutrition.
Call Our Office
This sheet is not intended to substitute for our care, nor prevent telephone communication as needed. Any child with gastroenteritis who is under two years of age, or has fever over 102°F, headache, severe abdominal pain, or signs of dehydration should be brought to our attention immediately. Also call our office if:
-
Vomiting or diarrhea increases in severity (not keeping any fluids down).
-
Vomiting continues after 24 hours on a clear liquid diet.
-
Diarrhea has not improved after four days.
-
The child starts to vomit blood or pass blood in the stools.
-
The child develops excessive irritability.
-
The child is not urinating as much, is not making at least 3 wet diapers per day, or is showing other signs of dehydration.
Ear Infection
Description
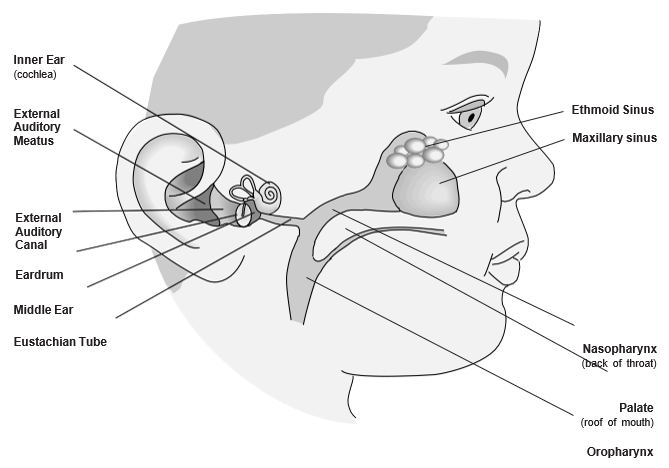
An ear infection is a bacterial infection of the middle ear (the space behind the eardrum). It usually is
caused by a cold, occurring after the cold blocks off the eustachian tube (the passage connecting the middle ear to the back of the throat), which allows bacteria to grow in this space. The ear is painful because trapped, infected fluid puts pressure on the eardrum, causing it to bulge. Other symptoms are irritability, poor sleep, and fever.
Most children will have at least one ear infection, and over three quarters of these children will have repeated ear infections. In a few cases, the pressure in the middle ear causes the eardrum to rupture and drain. This small tear usually heals within one week.
Home Treatment
Antibiotics
Your child may be treated with an antibiotic for 10 days. This medicine will kill the bacteria that are causing the ear infection. Even though your child will feel better in a few days, give the antibiotic until it is all gone or as instructed by your doctor. If your child does not feel better after a few days of antibiotics, contact your child’s doctor.
Pain Relief
-
Acetaminophen (Tylenol®) or ibuprofen (Motrin, Advil) can be used to help with the earache or fever for a few days until the antibiotic takes effect.
-
For severe pain, try elevating your child’s head when sleeping.
-
Placing a warm washcloth over the infected ear for a few minutes may help decrease the pain.
Restrictions
Your child may go outside and does not need to cover his/her ears. Swimming is permitted as long as there is no perforation (tear) in the eardrum or drainage from the ear. Air travel or
a trip to the mountains is safe _ just have your
child swallow fluids, suck on a pacifier, or chew during ascent and descent. Ear infections are not contagious.
Ear Recheck
We generally schedule a return appointment in two to twelve weeks for children under 2 years old, or for certain children over 2 years old with language or learning problems or with frequent ear infections. We will look at the eardrum to be certain that the infection has cleared up and more treatment isn’t needed.
Call Our Office Immediately If:
-
Your child develops a stiff neck.
-
You feel your child is getting worse.
-
There is blood or pus draining from the ear canal.
-
The fever or pain is not gone after your child has taken the antibiotic for 48 hours.
Adapted from B.D. Schmitt, M.D., “Your Child’s Health,” Bantam Books. Copyright 1994 Clinical Reference Systems, Ltd.
Fever in Children
What Is Fever?
Fever is the body’s normal response to infections and may be helpful in fighting them. When white blood cells attack germs, they release chemical signals which cause the brain to elevate the temperature. This elevation may help the body kill the germs faster. The usual fevers (100°F to 104°F) that all children get are not harmful. Most are due to viral illnesses; some are due to bacterial ones. Teething does not cause fever.
The symptoms and characteristics of fever include a rectal temperature over 100.4°F (38.0°C), oral temperature over 100°F (37.8°C), and axillary (armpit) temperature over 99°F (37.2°C). While the body’s average temperature is 98.6°F (37°C), it fluctuates from a low of 97.6°F in the morning to a high of 100°F in the late afternoon. Mild elevations of temperature can be caused by exercise, excessive clothing, hot weather, or warm food or drink. If you suspect one of these causes, retake the temperature after 30 minutes.
How Do You Take Temperatures?
Use digital, not mercury, thermometers because they are safer, faster, and more accurate. For children under five years of age, use axillary or rectal measurements. Most children four or five and older are ready for oral readings. Ear thermometers may be unreliable, especially in children under one year old. In young children, high ear thermometer readings should be confirmed by another method. Axillary: Place the tip of the thermometer in a dry armpit and close the armpit by holding the elbow against the chest. If you’re uncertain about the result, check it with a rectal thermometer.
Rectal: Place your child stomach-down on your lap, or on his back on a changing table. Lubricate the end of the thermometer and the opening of the anus with petroleum jelly (Vaseline or KY Jelly). Carefully insert the thermometer about one inch, but never force it. Hold the child still and rest your hand on the buttocks to stabilize the thermometer.
Oral: Be sure your child has not recently taken a cold or hot drink. Place the tip of the thermometer underneath the tongue on either side, rather than at the front of the mouth. The child should hold it in place with the lips and fingers (not the teeth), keeping the mouth closed and breathing through the nose. If the nose is congested, take an axillary temperature.
You do not need to check your child's temperature if he is not sick, or many times a day when he is sick. Remember that the main purpose of temperature-taking is to determine if a fever is present, not to chart its every move.
How Long Does Fever Last?
Most fevers associated with viral illness range between 101°F and 104°F and last for one to three days. In general, the height of the fever isn’t related to the seriousness of the illness. What counts is how sick your child acts. With most infections, the level of fever bounces around for two or three days. Shivering or feeling cold indicates that the fever has peaked; sweating means it is coming down. It is important to understand that there is no evidence that fever itself can be harmful unless the temperature exceeds 107°F. Fortunately, the brain’s thermostat keeps nearly all untreated fevers below this level. A small number of young children may develop convulsions (seizures) with fever. While these are frightening, they do not appear to cause harm and are not usually a sign of more serious illness. Still, call your child's doctor if your child has a febrile seizure.
When Should I Call?
If your child is under three months old, call us day or night if the rectal temperature is greater than 100.4°F. Beyond three months, call immediately if the fever is over 105°F, your child is crying inconsolably or whimpering, or cries if you touch or move him. Also call immediately if the child’s neck is stiff, any purple spots are present on the skin, breathing is difficult and no better after you clear the nose, or a convulsion (seizure) has occurred. Call if burning or pain occurs with urination. Also call if your child is under two years of age and has a fever of 104°F or greater. Call if the fever has been present more than 72 hours, more than 24 hours without obvious cause, or has returned after going away for more than 24 hours.
Which Medications Should I Use?
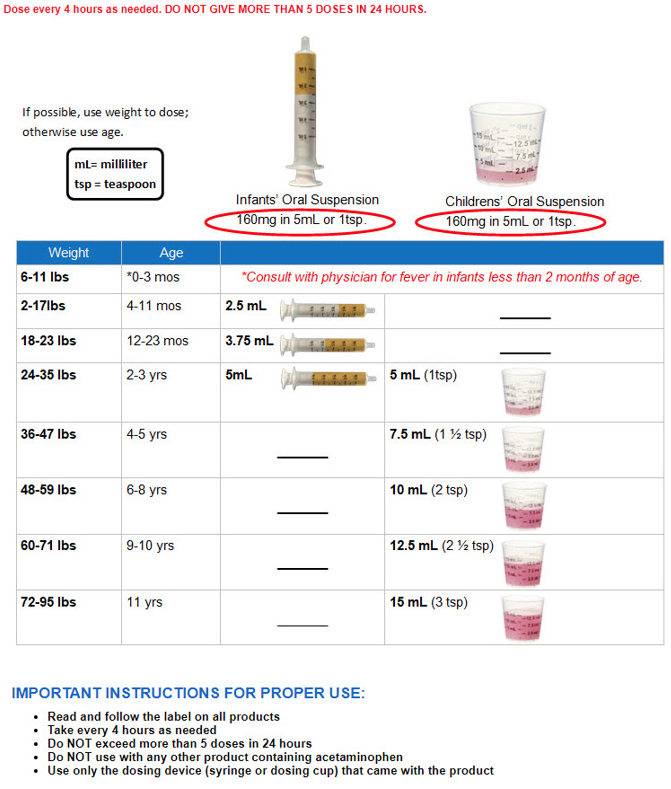
Check with our office before using medication for children under four months of age. Children of any age can be given acetaminophen (Tylenol®, Tempra®, Liquiprin®, Panadol®) if the fever is causing discomfort. Acetaminophen will reduce the fever but usually not bring it down to normal and the fever may recur after the aceteminophen wears off. Liquid ibuprofen (Advil, Motrin®) may also help improve comfort and reduce the temperature in feverish children and can be given to infants six months or older. See chart that follows for dosing. If your child is sleeping, don't awaken him for medications, and do not use them for more than three days without consulting your pediatrician.
Other Measures to Take:
Encourage, but don’t force, extra fluids. Popsicles and iced drinks may help replace body fluids lost because of sweating. Keep clothing to a minimum because most heat is lost through the skin. Bundling up your child will cause a higher fever. Be especially careful of infants, who cannot undress themselves if they become overheated. If your child feels cold or is shivering, use a light blanket. Discourage vigorous activities because they produce additional heat. Normal play, however, is perfectly fine.
A Word of Caution About Aspirin
The American Academy of Pediatrics and other health organizations have recommended that patients through 21 years of age not receive aspirin if they have chickenpox or influenza (any cold, cough, or sore throat symptoms). Several studies have linked aspirin to Reye’s syndrome, a severe illness that resembles encephalitis. Many pediatricians have stopped using aspirin for fevers associated with any illness because it has the potential to be so dangerous.
Medicines and Dosages to Reduce Pain and Fever
Choose the proper medicine, and measure the dose accurately
-
Always use a proper measuring device. For example: When giving acetaminophen liquid (e.g., Tylenol), use the device enclosed in the package. If you misplace the device, consult your healthcare provider or pharmacist for advice. Kitchen spoons are not accurate measures. When giving ibuprofen liquid (e.g., Advil, Motrin), use the device enclosed in the package. Never use a kitchen spoon!
Take these two steps to avoid causing a serious medication overdose in your children
Don’t give your child a larger amount of acetaminophen (e.g., Tylenol) or ibuprofen (e.g., Motrin, Advil) than is shown in the table below. Too much of any of these medicines can cause an overdose.
When you give your child acetaminophen or ibuprofen, don’t also give them over-the-counter (OTC) cough or cold medicines. This can also cause a medication overdose because cough and cold medicines often contain acetaminophen or ibuprofen. In fact, to be safe, don’t give OTC cough and cold medicines to your child unless you talk to your child’s healthcare provider first.
Pediatric Ibuprofen
Dosing Instructions for Infants and Children
Pediatric Acetaminophen
Dosing Instructions for Infants and Children
|